Diabetic medications and major congenital malformations
4.5 (280) · $ 35.00 · In stock
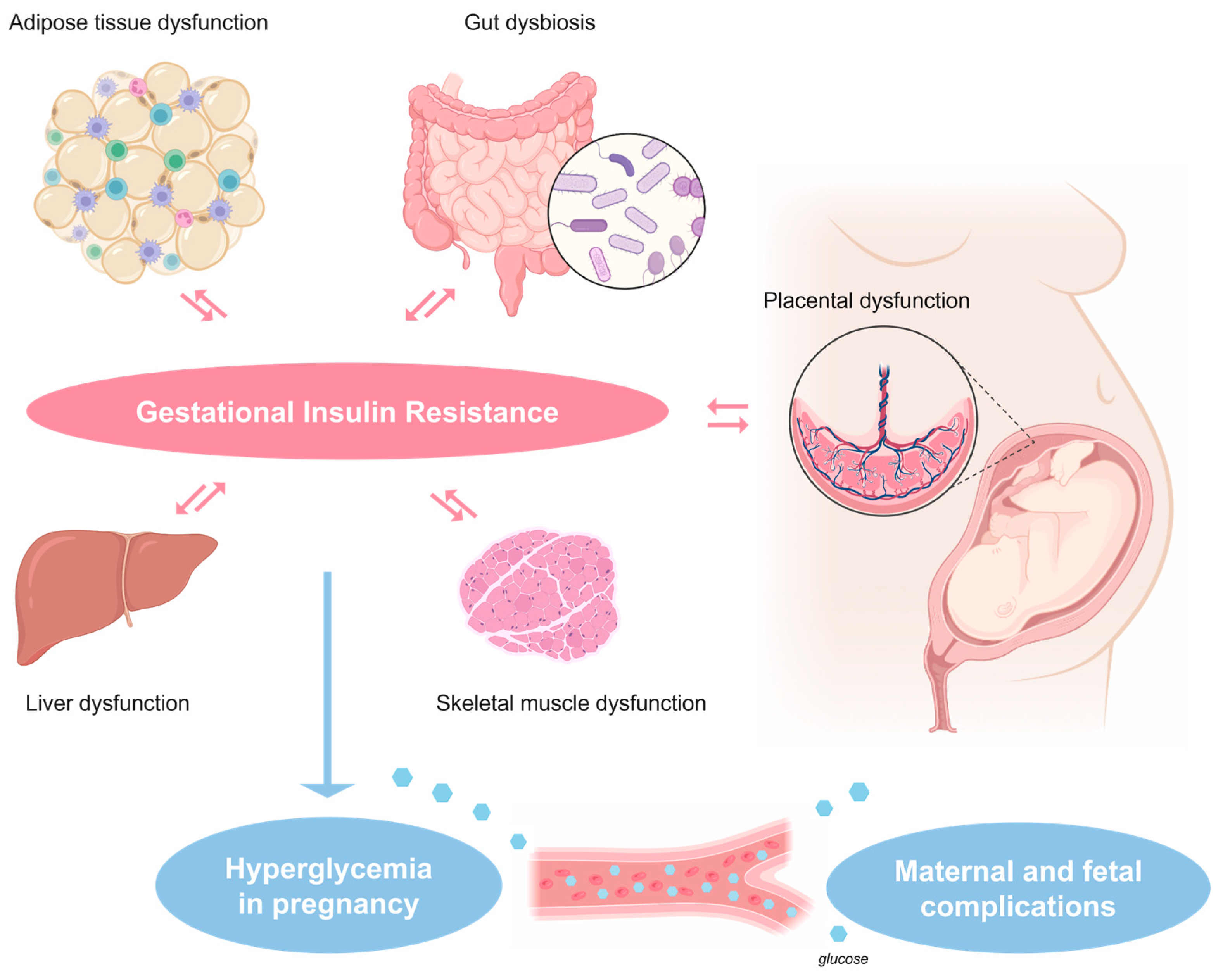
ABSTRACT The global prevalence of type 2 diabetes mellitus (T2DM) is increasing. T2DM is more common in patients with psychiatric disorders and those who take certain psychotropic drugs. T2DM occurs in 2%–7% of women of reproductive age. The prevalence of pregestational diabetes is 0.5%–2.4%, and that of gestational diabetes is 7%–28%, depending on geographical region. About 20%–50% of pregnancies, across the world, are unplanned; this figure is higher, at about 65%, in women with psychiatric disorders. As a result, many women of reproductive age who have diabetes, including women who do not know that they have diabetes, may unintentionally become pregnant, thus unknowingly exposing their pregnancy to diabetes and its treatment. Exposure of pregnancy to pregestational and gestational diabetes is associated with risks to the mother as well as risks to the child. Risks to the mother include obesity, hypertension, and preeclampsia. Risks to the child include spontaneous abortion, fetal death, macrosomia, major congenital malformations (MCMs), preterm delivery, neonatal hypoglycemia, neonatal hyperbilirubinemia, and neonatal respiratory distress syndrome. A recent large retrospective cohort study with data from 6 countries in Europe, Asia, and North America found that, in about 51,000 women with pregestational T2DM, neither MCMs nor cardiac malformations were more prevalent in offspring of children periconceptionally exposed to second-line antidiabetic treatments relative to exposure to insulin. These findings are reassuring but have limitations that are discussed. A reasonable conclusion from a reading of the reviewed literature is that pregestational and gestational diabetes are best treated during pregnancy, that insulin is a first-line treatment, that metformin is an increasingly accepted alternative, and that safety data on second-line antidiabetic treatments are, so far, reassuring. J Clin Psychiatry 2024;85(1):24f15318 Author affiliations appear at the end of this article

Neonatal Care of the Infant of the Diabetic Mother
Pharmaceuticals, Free Full-Text
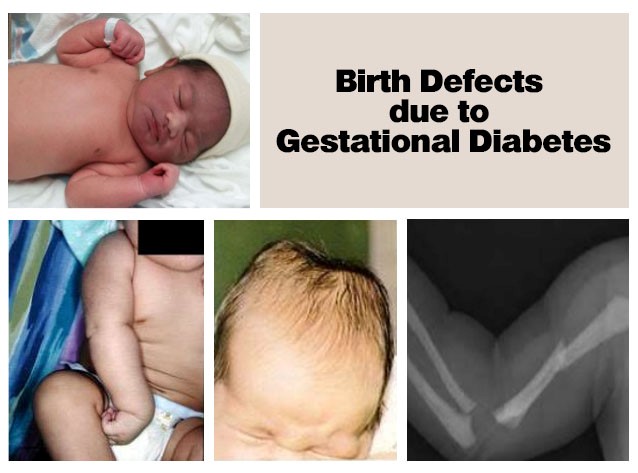
Birth Defects due to Gestational Diabetes

Trajectories in Cerebral Blood Flow Following Antidepressant Treatment in Late-Life Depression: Support for the Vascular Depression Hypothesis

Multisite, Randomized, Double-Blind, Placebo-Controlled Pilot Clinical Trial to Evaluate the Efficacy of Buspirone as a Relapse-Prevention Treatment for Cocaine Dependence

ARVCF Genetic Influences on Neurocognitive and Neuroanatomical Intermediate Phenotypes in Chinese Patients With Schizophrenia

Gestational diabetes is associated with the risk of offspring's

Gestational diabetes - Wikipedia

Childhood Adversity and Schizophrenia: The Protective Role of Resilience in Mental and Physical Health and Metabolic Markers

Psychosocial Implications of Tardive Dyskinesia in Patients With Mood Disorders Versus Schizophrenia
Diabetology, Free Full-Text
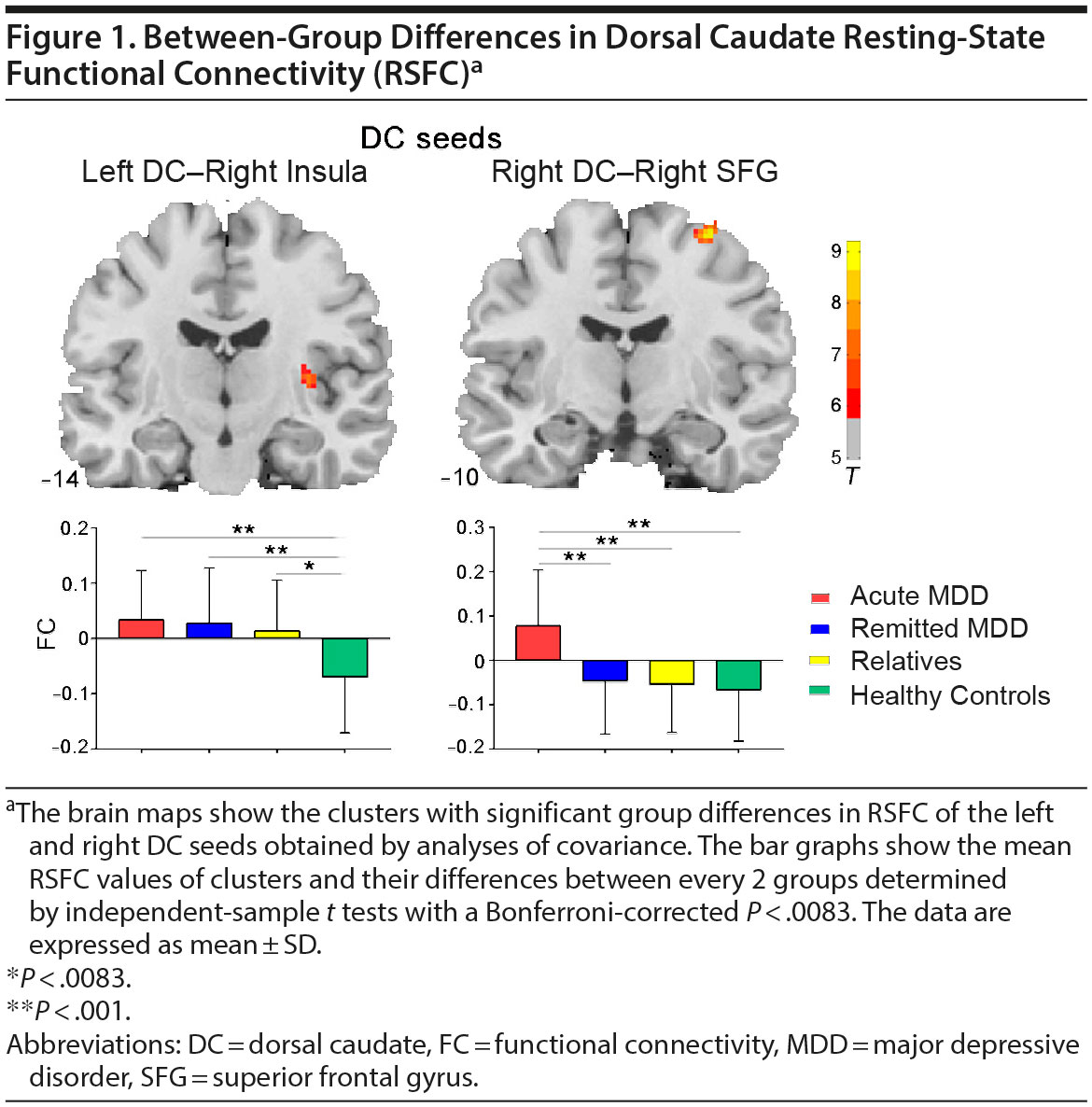
Striatal Resting-State Connectivity Abnormalities Associated With Different Clinical Stages of Major Depressive Disorder
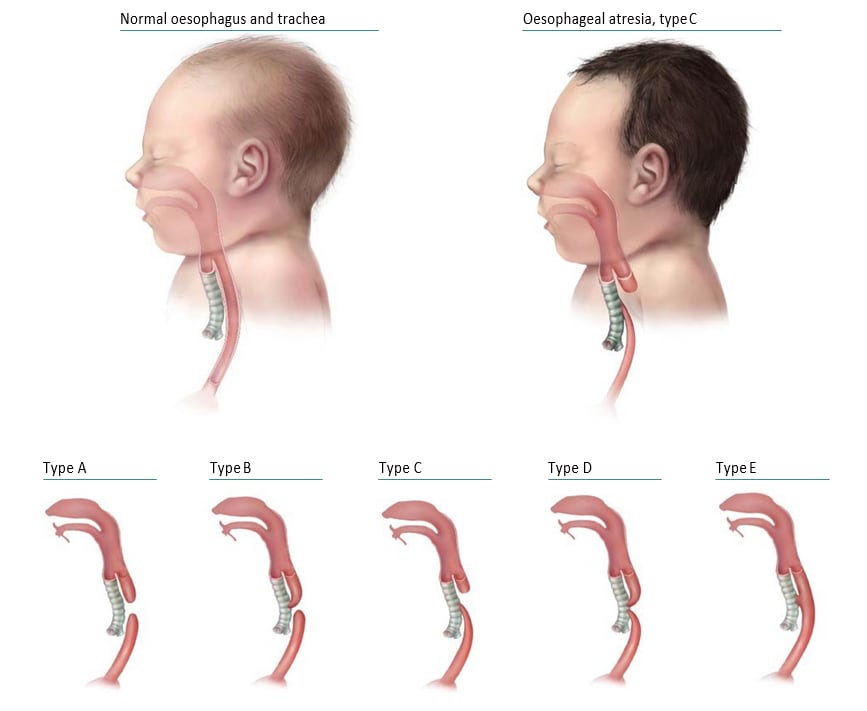
Surveillance Manual - 4.7 Congenital malformations of the digestive system

Does Fathers' Diabetes Increase the Risk of Birth Defects on Babies?












